Discover Our
Latest Posts
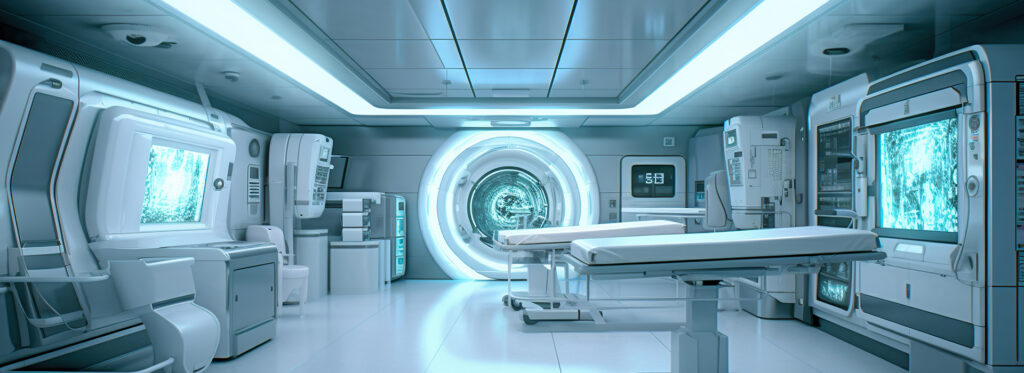
Artificial Intelligence is transforming the field of teleradiology and enhancing its precision and efficiency. AI’s integration into this domain promises improvements in diagnostic accuracy, workflow efficiency, and overall accessibility, thus enhancing the patient outcomes and revolutionizing the delivery of services in healthcare.
One of the most significant contributions of AI in teleradiology is its ability to enhance diagnostic accuracy. Traditional teleradiology depends heavily on the expertise of radiologists, who remotely interpret a vast array of images. However, chances of human error are there, particularly when radiologists are overwhelmed with high volumes of studies or when interpreting subtle abnormalities. AI algorithms, especially those based on deep learning, can analyse medical images with remarkable precision. Trained on large datasets, these AI models can detect patterns and anomalies that may escape human eyes, providing a second layer of scrutiny. Studies have shown that AI can match or even surpass human radiologists in identifying conditions like lung nodules, breast cancer, and neurological disorders. By flagging suspicious findings and highlighting areas of concern, AI helps the radiologists in making more accurate diagnoses, thus, reducing the likelihood of errors and improving the outcome of patient care.
Efficiency is another domain where AI significantly impacts teleradiology. Radiologists often face the challenge of interpreting a large number of imaging studies within shorter time frames especially in ER cases, which can delay diagnosis and treatment. AI-powered tools can streamline this process by quickly analysing images and providing preliminary reports. These tools can prioritize cases based on the severity of findings, ensuring that urgent cases receive immediate attention. For example, AI algorithms can detect critical conditions like intracranial haemorrhages or pulmonary embolisms and alert radiologists, enabling swift intervention. This capability not only speeds up the diagnostic process but also optimizes radiologists workflow, allowing them to focus on complex cases that requires their expertise.
AI’s role in image enhancement and reconstruction further strengthens its benefits in teleradiology. Images acquired from remote may often be of lower quality due to limitations in imaging equipment or transmission issues. AI algorithms can enhance these images by reducing noise, correcting artifacts, and improving resolution, ensuring that the radiologists receive clear and accurate images for interpretation. This capability is especially necessary in teleradiology, where the quality of transmitted images can directly impact the diagnostic decisions.
Another significant advantage of AI in teleradiology is its potential to provide access to high-quality radiological services. In many regions, particularly in rural areas, access to specialized radiologists is limited. AI can bridge this gap by providing diagnostic support to healthcare providers in these areas. AI algorithms can perform initial image assessments and generate diagnostic reports, which can then be reviewed by remote radiologists. This collaborative approach ensures that patients in remote locations receive timely and accurate diagnoses, thus improving access to essential healthcare services.
The integration of AI into teleradiology also holds promise for advancing personalized medicine. By analysing imaging data alongside other clinical information, such as EHR and genomic data, AI can provide comprehensive insights into a patient’s condition and can predict a patient’s response to specific treatments based on imaging features and clinical history, allowing for personalized therapeutic strategies that improve patient outcomes.
Despite its numerous advantages, the adoption of AI in teleradiology comes with challenges. Ensuring the accuracy and reliability of AI algorithms is paramount, as errors can have serious implications for patient care. Robust validation and continuous monitoring of AI tools are necessary to maintain high standards of diagnostic performance. Additionally, ethical considerations related to data privacy and algorithmic bias must be addressed. Collaborative efforts among radiologists, AI developers, and regulatory bodies are essential to overcome these challenges and establish guidelines for the safe and effective use of AI in teleradiology.
Artificial Intelligence has been transforming diagnostic imaging by enhancing the accuracy, efficiency, and accessibility of radiological practices. The integration of AI into this domain has opened new paths for improving patient outcomes, reducing healthcare costs along with addressing the growing demand for medical imaging services.
One of the most significant contributions of AI in diagnostic imaging is its ability to enhance image interpretation. Traditional radiology is highly dependent on the expertise and experience of radiologists, who must meticulously analyse images to detect abnormalities. AI, particularly deep learning algorithms has been assisting radiologists by automatically identifying and highlighting areas of concern, thereby reducing the likelihood of human error. These algorithms are trained on large datasets of annotated medical images, allowing them to recognize complex patterns and anomalies that might get missed by the human eye. For instance, AI algorithms have showed remarkable accuracy in detecting conditions such as lung cancer, breast cancer, and intracranial haemorrhages, often matching or even sometimes surpassing the performance of radiologists.
Furthermore, AI can significantly speed up the diagnostic process. Radiologists are often burdened with large volumes of imaging studies, leading to delays in diagnosis and treatment. AI-powered tools can process and analyse the images quickly, providing preliminary assessments that can expedite clinical decision-making. This is particularly beneficial in emergency settings where timely diagnosis is critical. By prioritizing those cases that require immediate attention, AI can help ensure that patients receive prompt and appropriate care.
Another key advantage of AI in diagnostic imaging is its potential to standardize the radiological interpretations. Most of the times, different radiologists provide differing opinions on the same imaging study. AI algorithms, being consistent and objective, can reduce this variability and provide standardized assessments. This is especially valuable in regions with limited access to expert radiologists. AI can bridge the gap by providing high-quality diagnostic support to healthcare providers in remote areas, thereby improving access to medical imaging services.
AI’s role in diagnostic imaging extends beyond mere image interpretation. It also comprehends image acquisition and reconstruction. In modalities like MRI and CT, AI can optimize scanning protocols to reduce scan times and minimize radiation exposure without compromising image quality. Advanced AI techniques can increase image resolution and clarity, enabling more accurate diagnoses from lower-quality images. This is particularly important in pediatric and other vulnerable populations where it is critical to minimize the radiation exposure.
Additionally, AI can integrate imaging data with other clinical information to provide comprehensive insights into a patient’s health. By combining radiological findings with electronic health records, laboratory results, and genomic data, AI can offer a complete view of the patient’s condition. This integration facilitates personalized medicine, where treatment plans are tailored to the individual’s unique characteristics and disease profile. For example, AI can predict a patient’s response to a particular therapy based on imaging and clinical data, allowing more targeted and effective interventions.
Despite its immense potential, the use of AI in diagnostic imaging is not without challenges. Ensuring the accuracy and reliability of AI algorithms is of high importance, as errors can have serious implications for patient care. Robust validation and rigorous regulatory oversight are necessary to build trust in AI-driven diagnostic tools. Additionally, there are ethical considerations related to data privacy and algorithmic bias. AI systems must be designed to protect patient confidentiality and avoid biases that could lead to disparities in care.
In conclusion, AI is poised to transform diagnostic imaging by complementing radiologist’s capabilities, accelerating the diagnostic process, and enabling access to high-quality imaging services. As technology continues to advance, AI’s integration into diagnostic imaging holds the promise of more accurate, efficient, and personalized patient care. Embracing this innovation requires collaboration among radiologists, AI developers, and regulatory bodies to ensure that AI’s potential is fully realized while safeguarding the patient safety and ethical standards.
Connect
USA Office
- 228 Park Ave S, PMB 20522 New York, NY 10003
- connect@gyriz.trio-spire.com
- Office Number: (607) 408 5050
UK Office
- Bridge Road Innovation Centre Camberley Surrey GU15 2QR
- connect@gyriz.trio-spire.com
Ireland Office
- Alexandra House Ballsbridge, Dublin 4 D04 C7H2
- connect@gyriz.trio-spire.com
Poland Office
- Stefana Batorego 1, 31-135 Kraków
- connect@gyriz.trio-spire.com